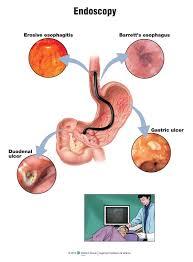
What is Interventional Endoscopy?
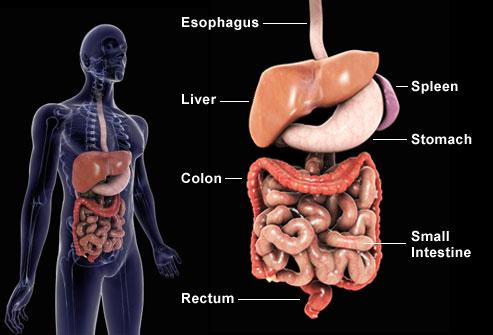
Interventional Endoscopy encompasses a variety of endoscopic procedures used to diagnose and treat diseases that are typically beyond the scope of regular endoscopic techniques. By combining advanced imaging and device technology with technical expertise, our physicians are helping patients to avoid more invasive traditional treatment approaches such as surgery. These procedures are minimally invasive, meaning they are performed using thin flexible tubes advanced through the body's natural orifices such as the mouth and rectum, thus avoiding the complications associated with surgery and providing faster recovery times. Interventional endoscopy is utilized in the treatment of bile duct stones, stenting of the gastrointestinal tract, treatment of gastrointestinal bleeding, and the diagnosis and treatment of tumors involving the esophagus, stomach, biliary system, pancreas, small bowel and colon. The procedures are typically performed on an outpatient basis, and most patients may return home the same day.
Endoscopic Procedures
Argon Plasma Coagulation (APC)
Argon plasma coagulation uses ionized argon gas passed through a catheter within an endoscope to deliver electrical current to gastrointestinal lesions. The delivered energy results in superficial coagulation of the target tissue. APC is used to treat bleeding lesions such as vascular malformations, or to debulk tumors within the GI tract.
Capsule Endoscopy
Video Capsule Endoscopy utilizes a miniature camera approximately the size of a large pill that is used to take pictures of the small bowel normally beyond the reach of regular endoscopes. After the camera is swallowed, it begins to take pictures of the bowel at regular intervals. The picture data is continuously delivered to a recording device worn as a belt. At the end of the procedure day, the belt is returned and the data are uploaded to a computer for review by a physician. Capsule endoscopy can be used to identify sources of blood loss from the GI tract, tumors or polyps of the small bowel, and assess for inflammatory conditions such as Crohn's disease.
Celiac Plexus Blockade/Neurolysis
Celiac Plexus Blockade and Neurolysis are used to relieve pain associated with chronic pancreatitis and pancreatic cancer. Endoscopic ultrasound (EUS) is used to identify the celiac plexus, a network of neural tissue that modulates the sensation of pain felt from pancreatic injury. Using a small needle advanced under real-time EUS guidance, a physician delivers agents to interrupt the pain signals that pass through the celiac plexus, thus providing pain relief to patients. Following the procedure, patients may often reduce their use of narcotics, thereby improving their quality of life and energy levels. These procedures can be performed as an outpatient, and you can return home the same day.
Choledochoscopy
Blockage of the bile duct may be caused by large stones or tumors that may be difficult to treat. Choledochoscopy utilizes a miniature endoscope that is passed through a regular endoscope and up into the biliary tree. Choledochoscopy provides direct visualization of the bile ducts, allowing for targeted biopsies of bile duct strictures and tumors. Local therapies may also be delivered, including electrohydraulic lithotripsy for the treatment of large, recalcitrant stones.
Chromoendoscopy
Precancerous lesions and early-stage tumors are often difficult to detect visually during traditional endoscopy, leading to missed diagnoses. Chromoendoscopy utilizes specialized light filters and dyes to enhance the appearance of superficial mucosal architecture and blood vessels resulting in improved detection of early cancers.
Cryotherapy
Cryotherapy uses extreme cold to ablate diseased tissue in the GI tract. Liquid nitrogen or carbon dioxide is delivered using a catheter passed through an endoscope to freeze the target tissue. Cryotherapy has been used in the treatment of Barrett's esophagus and esophageal cancer.
Drainage of Pancreatic Pseudocysts
Pseudocyst drainage is performed using endoscopic ultrasound (EUS) to visualize the lesion from the stomach or duodenum. A thin needle is then used to puncture the cyst. Under fluoroscopic guidance, drainage catheters are then placed into the cavity, allowing for further drainage over time, and eventual healing of the cavity.
Ductoscopy
Ductoscopy utilizes a miniaturized endoscope that is passed through the working channel of a regular endoscope to examine the bile or pancreatic ducts. Targeted biopsies or lithotripsy may be performed.
Endoclipping
Endoclips are small metallic devices used to treat bleeding lesions such as ulcers, vascular malformations, and mucosal defects such as perforations or fistulas. The clips are delivered through an endoscope, and once deployed remain in place for several days to weeks. Once the mucosa heals, the clips will spontaneously detach and pass undetected in the stool.
Endoscopic Mucosal Resection (EMR)
EMR encompasses the removal of precancerous and early gastrointestinal tumors using minimally invasive endoscopic techniques. EMR is currently used to remove tumors of the esophagus, stomach and colon/rectum, along with Barrett's esophagus and colon polyps. EMR can be used to avoid surgical treatment of these lesions.
Endoscopic Retrograde Cholangiopancreatography (ERCP)
ERCP is an advanced endoscopic technique used to examine the biliary and pancreatic ducts. Small catheters are passed through the endoscope into the ducts, and x-rays are used to obtain images of the ductal anatomy. ERCP is used to remove stones, diagnose and treat Sphincter of Oddi Dysfunction, treat strictures using dilation balloons and catheters, and place stents to facilitate drainage of bile and pancreatic juices. ERCP can be combined with choledochoscopy and EUS to perform additional therapeutic maneuvers.
Endoscopic Ultrasound (EUS)
EUS combines traditional endoscopy with ultrasound imaging to visualize structures within the wall of the GI tract and beyond. A miniature ultrasound transducer is housed at the tip of an endoscope, allowing for visualization of a broad range of structures from the esophagus to rectum. From within the esophagus, the mediastinum and associated lymph nodes can be seen, and diseased nodes can be sampled using fine-needle aspiration (FNA). From the stomach and duodenum, the abdominal vessels can be identified, along with nearly all the organs of the abdomen including the liver, bile ducts, pancreas, spleen, adrenal glands, and kidneys. FNA is often performed, and interventional EUS drainage procedures such as pseudocyst drainage are possible. From the rectum and colon, tumors colorectal cancers can be staged, and disorders of the anorectal sphincter complex can be diagnosed. Throughout the GI tract, lesions arising from within the wall of the GI tract (submucosal tumors) can be characterized by EUS, and tissue can be obtained via FNA for diagnosis.
Enteral Stenting
Processes such as advanced tumors, radiation therapy, gastroesophageal reflux (GERD), and gastrointestinal surgery may result in symptomatic narrowing of the GI tract leading to problems such as obstruction, pain, vomiting and malnutrition. Enteral stents are used to restore and maintain patency of the GI tract. They are either plastic or metal fibers arranged in a tubular meshwork, and come in removable or permanent varieties.
Enteroscopy
Enteroscopy is the endoscopic evaluation of the small bowel using specialized endoscopes. Traditional endoscopes and colonoscopes are only able to evaluate a limited length of the beginning and end of the GI tract. Deep enteroscopy uses specialized equipment navigate through the length of the small bowel to evaluate sources of bleeding or treat polyps and tumors.
Lithotripsy
Lithotripsy is used to fracture and dissolve large recalcitrant obstructing stones of the bile or pancreatic ducts. Several techniques are available, including electrohydraulic, extracorporeal shock-wave lithotripsy, and laser lithotripsy. The choice of technique normally dictated by the type of stone and its location. This procedure can be repeated until the stone is dissolved.
Radiofrequency Ablation (RFA)
RFA is a thermal ablative technique that utilizes current that is delivered through a balloon catheter or probe to treat Barrett's esophagus and early esophageal cancer. RFA is a safe, minimally invasive treatment that may prevent the need for esophageal surgery. This procedure can be performed as a come-and-go procedure.
Resection of Colonic Polyps
Colon polyps are precancerous growths that develop due to a variety of factors. When polyps become very large, the associated risk of developing cancer increases, and the polyp may be difficult to resect using traditional methods. Large polyps may be removed using a combination of mucosal resection techniques.
Stone Extraction
Stones are concretions that develop within the biliary tree or pancreatic ducts. Stones may cause obstruction leading to pain and occasionally, a life threatening infection known as cholangitis. Stones are extracted during ERCP using extraction baskets and/or balloons. Lithotripsy and choledochoscopy may be used to extract large stones.
Stricture Dilation
A stricture is a symptomatic narrowing in the GI tract that may cause symptoms of obstruction including abdominal pain, bloating, nausea, vomiting, and malnutrition. Dilation is performed using specialized balloons that gradually stretch the narrowed area during an endoscopy. High-grade strictures may require serial endoscopic dilations that are performed on an outpatient basis.
Zenker's Diverticulum Septotomy
A specialized needle knife is used to incise the septum of the diverticulum thus relieving the dysphagia, or difficulty swallowing associated with this condition.